
The Natural fit
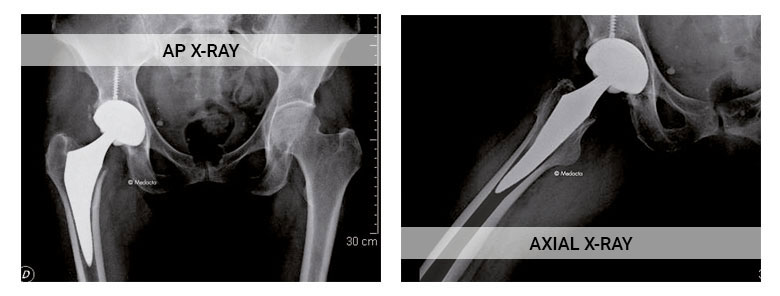
The philosophy of anatomical stems was introduced into the market during the 1980's with the aim to obtain the best press-fit in the metaphyseal femur using a design following the natural geometry of the proximal femur. The MiniMAX is an anatomical cementless stem engineered to provide the best fit and fill in the metaphyseal femur following the natural shape of the femoral canal. [1,2] The length of the stem and the shape have been studied size by size and have shown to be bone preserving and to provide good mechanical stability. [3]


9° anteversion.
Mirror polished with 12/14 Eurocone taper.
Growing size by size to restore anatomy.

The best fit and fill in the metaphysis to restore physiological loads.
127° neck-shaft angle.

Negative medially and positive laterally:

Rounded and non invasive:
Providing minimal risk of impingement and fracture.
Making the insertion of the stem in the femoral canal easier.

Short and thin with 5° curvature and a distal optimisation:

MiniMAX is made of Titanium-Niobium alloy (Ti-6Al-7Nb).
The surface treatment consists of:
The HA coating has chemical characteristics similar to that of the human bone which stimulates the bony ongrowth [4,5,6,7].
When all of the HA coating is absorbed there is good interaction between stem and bone leading to long-term stability.
The MiniMAX stem is available in 9 sizes, from 0 to 8 in both left and right versions.

The anterior approach, strengthened by several years of clinical experience, is the only technique which follows a path both intermuscular and internervous and therefore reduces considerably the risk of damaging periarticular structures such as muscles, tendons, vessels and nerves.
Thanks to its expertise, unique in the market, Medacta International is the worldwide leader for Anterior Minimally Invasive Surgery (AMIS) with worldwide learning centers to teach the surgical approach, permanent support for surgeons and continuous development of specific instrumentation.
With the use of MiniMAX you can enter the Medacta International AMIS world.

Discover:
[1] Noble PC, Alexander JW et al. The Anatomical Basis of Femoral Component Design. Clin Orthop. 1988; 235: 146-65.
[2] Husmann O, Rubin PJ et al. Three-dimensional Morphology of the Proximal Femur. J Arthroplasty. 1997; 12(4): 444-50.
[3] Data on file: Medacta.
[4] Hardy et al. Bonding of Hydroxyapatite Coated Femoral Prostheses JBJS vol 73-B, No5, Sept. 1991.
[5] Hardy et al. Aspects Radiologiques de l’Arthroplastie Fémorale Revetue d’Hydroxyapatite et correspondence Histologiques Acta Orthop. Bel. Vol 59, Suppl I, 1993.
[6] Hardy et al. Projection d’Hydroxyapatite sur Prothèses Articulaires : Progrès ou Illusion ? Acta Orthop. Bel. Vol 59, Suppl I, 1993.
[7] Fraissinet P, Hardy D et al. Histological analysis of the bone-prosthesis interface after implantation in humans of prostheses coated with hydroxyapatite. The journal of Orthop Surg. 1993; 7(3): 246-53.